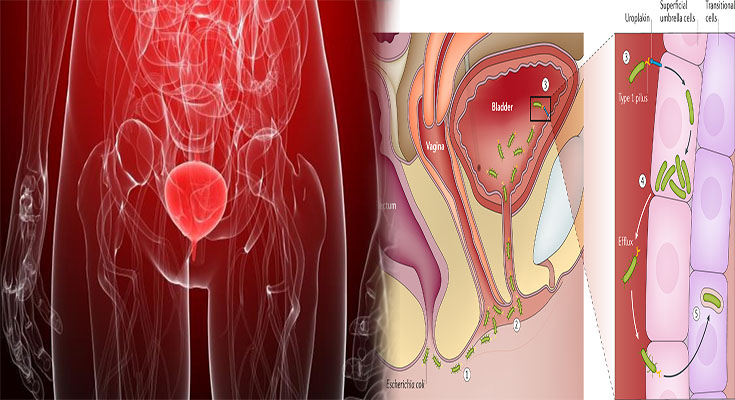
Interstitial cystitis (IC), also known as painful bladder syndrome, is a chronic condition that causes recurring pain in your bladder and pelvic area. Many people with IC also experience urinary urgency, pelvic pain and pressure, frequent urination and urinary tract infections.
While there’s no cure for IC, treatments can help reduce symptoms and make life easier to live. Here are answers to common questions about interstitial cystitis.
What is Interstitial Cystitis?
Interstitial cystitis is a chronic condition that causes painful bladder syndrome. It’s also known as painful bladder syndrome, or IC/PBS for short.
Interstitial cystitis can cause inflammation and irritation in the lining of your bladder (the organ that stores urine). This can lead to frequent urination, pain or discomfort when you urinate, pelvic pain and pressure, blood in your urine or the feeling that you need to pee even when there’s nothing left in your bladder.
If you have interstitial cystitis symptoms but aren’t sure if they’re related to IC/PBS yet, this article will help explain what it is and how it affects people who have it.
What Are the Symptoms of Interstitial Cystitis?
Interstitial cystitis is a chronic condition characterized by pain in the bladder and pelvis. The symptoms can include:
- Pain in your bladder and pelvis, including:
- Pain with sex
- Pain after urinating or during urination (especially upon starting to pee)
- Frequent urination (more than 8 times per day) or urinary urgency (feeling like you have to go, even though you just went)
The severity of these symptoms varies from person to person; some people have mild discomfort while others experience extreme pain that interferes with their daily lives.
How Is Interstitial Cystitis Diagnosed and Treated?
To diagnose IC, your doctor will conduct a physical exam, order a urine test and perform a bladder scan. The diagnosis is made if there are signs of inflammation in the bladder wall.
The treatment for IC varies depending on the severity of symptoms as well as individual preferences. Treatment can be as simple as taking pain medications and antibiotics, or more complex with dietary changes and bladder retraining exercises.
How to Manage Painful Bladder Syndrome
To manage painful bladder syndrome, your doctor may recommend:
- Medications. The following medications can reduce the frequency and severity of your symptoms:
o Antibiotics. If you have a bacterial infection, your doctor will prescribe an antibiotic to treat it. Antibiotics are used to treat both acute and chronic interstitial cystitis (IC). These drugs work by killing bacteria that cause inflammation in the bladder wall or blockages in the ureters (the tubes that connect each kidney with its corresponding urethra). Doctors often prescribe these medications for several days at a time until all traces of bacteria are gone from your body; however, some people must take them long-term due to recurring infections
How to Treat Urinary Tract Infections
Urinary tract infections are common in women, and they can be treated with antibiotics. The best way to prevent them is through good hygiene and drinking plenty of water. If you have a UTI, it’s important that you take your medicine as prescribed by your doctor so that the infection doesn’t return or spread to other parts of your body. If recurrent UTIs are an issue for you, talk with a healthcare provider about ways they might be able to help reduce their frequency
Treatments are available for your painful bladder syndrome.
Treatments are available for your painful bladder syndrome.
- Medications: Your doctor may prescribe a medication to help you manage pain, such as ibuprofen or oxycodone. These drugs can help reduce inflammation and improve bladder function. However, they don’t cure IC/BPS or make it go away completely; they just relieve symptoms temporarily until the next flare-up occurs.
- Surgery: If medications aren’t working well enough or you have severe symptoms that affect your quality of life (for example, if you’re having trouble sleeping or doing everyday tasks), surgery might be an option for you. Surgery options include removing part of the bladder (partial cystectomy) or replacing part of your urethra with new tissue (urethral replacement). Both procedures can improve urine flow but won’t necessarily cure IC/BPS–it depends on what caused it in the first place! Surgery is usually only recommended when other treatments aren’t working well enough on their own because there are risks involved with any kind of procedure involving organs inside our bodies like this one does…
Interstitial cystitis is a condition that can cause bladder pain, frequent urination and bleeding from the urethra. It’s important to understand your options so that you can find the treatment that works best for you.